
Heart Device Answers
Welcome
Your source for information about heart devices, conditions, and more. If you have a specific question, type it into the search bar below to bring up content related to the topic.
Heart Device Answers was created to help answer your questions about heart devices and heart device therapies. The website is sponsored by Medtronic and some information is only applicable to Medtronic devices and patients in the United States. If you are a heart device patient, always refer to the product instructions and manuals applicable to your device. Talk to your healthcare provider about any symptoms you might have and whether these therapies might be right for you.

Your source for information about heart devices, conditions, and more. If you have a specific question, type it into the search bar below to bring up content related to the topic.


Cardiologists are doctors who specialize in the treatment of the cardiovascular system.

An ECG or EKG are interchangeable terms used to describe the recordings and tests that measure the electrical activity of the heart.

Cardiologists are doctors who specialize in the treatment of the cardiovascular system. An electrophysiologist is a cardiologist who specializes in the diagnosis and treatment of heart rhythm disorders.

A heart failure specialist is a cardiologist who specialize in treating heart failure.

The atria are the upper chambers of the heart that pump blood to the lower chambers (ventricles).

Cardiologists are often seen for possible issues with the heart. Seeing a cardiologist is often recommended for those experiencing chest pain, dizziness, and shortness of breath.

An EP is a cardiologist who specializes in the diagnosis and treatment of heart rhythm disorders.

SCA symptoms are immediate and dramatic and can include a loss of consciousness, sudden collapse, no breathing, and no pulse. Sometimes other symptoms can occur before a sudden cardiac arrest. These symptoms may include fatigue, fainting, blackouts, dizziness, chest pain, shortness of breath, weakness, palpitations, or vomiting. But sudden cardiac arrest can also occur with no warning.
Consult your doctor with any questions regarding any symptoms you may be experiencing and your medical condition.

Electrophysiologists (EP) are seen for electrical problems with the heart. Cardiac EPs are often recommended for patients whose heart rate is faster or slower than a normal pace or irregular instead of consistent.


Left ventricular dysfunction is when the heart is unable to maintain normal blood output due to a decrease in left ventricular function. This is characterized by a low ejection fraction.

SSS is a group of signs or symptoms that show that the heart's natural electrical pacemaker, the sinus node, is not working properly. With SSS, the heart rate can alternate between slow (bradycardia) and fast (tachycardia), often in combination with atrial fibrillation or atrial flutter. Treatment of SSS may involve a pacemaker and/or medication.

A rapid heart rate that starts in the ventricles. During VT, the heart does not have time to fill with enough blood between heartbeats to supply the entire body with sufficient blood. VT can be life threatening if it progresses to ventricular fibrillation.

SVT is as an irregularly fast or erratic heartbeat (arrhythmia) that affects the heart's upper chambers.

Tachycardia is a fast heart rate — more than 100 beats per minute while at rest — that can either start in the heart's lower or upper chambers. At these elevated rates, the heart is not able to efficiently pump oxygen-rich blood to the rest of the body.
Talk to a doctor to discuss causes, symptoms, risk factors, and potential treatment options.

AF or AFib is a common type of heart rhythm disorder affecting the atria, the upper chambers of the heart. It occurs when the atria quiver instead of contracting normally. Atrial fibrillation may increase a person's risk for stroke.

Bradycardia is a slow or irregular heart rhythm, usually fewer than 60 beats per minute. At this rate, the heart is not able to pump enough oxygen-rich blood to the body during normal activity or exercise.
Talk to a doctor to discuss causes, symptoms, risk factors, and potential treatment options.

The pericardium is a thin sac that surrounds the heart. It protects and lubricates the heart and keeps it in place within the chest.

Sinus tachycardia is a normal increase in heart rate that happens with fever, excitement, and exercise. Sinus tachycardia is normal, but treatment may be required if it is caused by an underlying problem, such as anemia (a low blood count) or hyperthyroidism (overactive thyroid gland), or rarely, happens frequently and without a clear cause (inappropriate sinus tachycardia).


An EP study is a procedure performed in a special lab in the hospital; the study attempts to reproduce an abnormal heart rhythm to diagnose arrhythmias.

Depending on a patient's heart condition, a pacemaker may help reduce shortness of breath by helping the heart beat normally. It's important to slowly return to normal activities and to report any issues, like shortness of breath, to the clinic. They may be able to re-program the pacemaker in a way that helps address shortness of breath.
Talk to a doctor about any additional concerns or questions.

An insertable cardiac monitor (ICM) is another name for an implantable heart monitor, injectable cardiac monitor, or loop recorder. An insertable cardiac monitor is a small medical device that can watch your heart for abnormal heart rhythms over time. It is sometimes called a loop recorder because it is continuously recording the heart rhythm, or on a loop. If it finds something abnormal, it saves the recording and sends it to the doctor or care team.
Specific components will vary depending on the type of device, but generally a heart device contains a battery, capacitor (the component of an ICD that stores and delivers charges) and electronics that control operation.

An extravascular ICD is an implantable cardioverter defibrillator where the device is placed under the skin below the left armpit, and the lead is placed outside the heart and veins.
Most implantable cardioverter defibrillators (ICD) have a method of stopping dangerous rhythms without a shock. This is called antitachycardia pacing, or ATP. ATP uses specifically timed pacing pulses to attempt to disrupt and end a dangerous rhythm allowing the heart to return to normal beating without a shock. Ask a doctor about ICDs with ATP functionality.
No, heart devices come in different shapes and sizes.
Typically, an ICD delivers between 20–40 joules per shock. Talk to a doctor or check with the device manufacturer to discuss programming settings that best fit individual needs.

These are different pacing modes your doctor can program for your device. This tells the device how to function when it comes to pacing and sensing. Each letter indicates something different (A = Atrium; V = Ventricle; D = Dual or both A and V; and O=none). The first letter indicates the chamber of the heart being paced. The second letter indicates the chamber of the heart being sensed or monitored. The third letter indicates how the device should respond when it senses a cardiac event (T = Triggered; I = Inhibited; D = Trigger or inhibit; and O = none). Finally, the fourth letter, usually “R,” means that the rate modulation function in the device is turned on (R = Rate modulation on; O or blank = none or no rate modulation). In this case DDDR means both the atrium and ventricle is paced, both the atrium and ventricle are sensed, the device can trigger or inhibit sensed events and rate modulation is turned on.

These are different pacing modes your doctor can program for your device. This tells the device how to function when it comes to pacing and sensing. Each letter indicates something different (A = Atrium; V = Ventricle; D = Dual or both A and V; and O = none). The first letter indicates the chamber of the heart being paced. The second letter indicates the chamber of the heart being sensed or monitored. The third letter indicates how the device should respond when it senses a cardiac event (T = Triggered; I = Inhibited; D = Trigger or Inhibit; and O = none). Finally, the fourth letter, usually “R,” means that the rate modulation function in the device is turned on (R = Rate modulation on; O or blank = none or no rate modulation). In this case DDD means both the atrium and ventricle is paced, both the atrium and ventricle are sensed, and the device can trigger or inhibit sensed events. A VVI mode means the pacemaker will pace in the ventricle, sense in the ventricle, and inhibit sensed events.


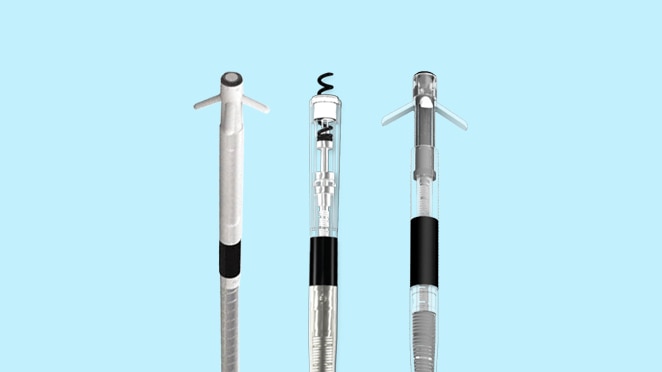
Most cardiac leads are attached to the inside of the heart wall with a small screw. However, there other attachment mechanisms depending on type of lead. Talk to a doctor with further questions on lead attachments.

After a heart device is implanted, the doctor may order tests such as an electrocardiogram (ECG), blood tests, or X-rays. These tests confirm that the lead is in the proper position inside the heart. Doctors may also recheck heart device settings to make sure they are providing the best treatment for specific heart conditions.
Following the implant, follow a doctor’s direction on restrictions and timelines to resuming normal activities.

It is common to have some soreness and tenderness at the incision site for several days after the procedure. There may also be some bruising. Healing of the incision is usually complete within 7 to 14 days. Because of this, a doctor may place restrictions on certain activities following surgery to allow for complete healing.
Consult with a doctor if experiencing any lingering pain.

In most heart device implants, an incision is made just below the collarbone. Then, leads are inserted and attached to the heart tested to make sure they are working properly. The leads are then connected to the device and everything is placed under the skin prior to closing up the incision and finishing the procedure.
Leadless pacemaker implants start with the insertion of a straw-like catheter system into a vein, typically near the upper thigh area of the leg. The catheter system moves the leadless pacemaker into the right ventricle of the heart where the device is placed against the heart wall and secured with flexible tines. The leadless pacemaker is tested to ensure it is working properly. The catheter system is then removed.
Leads are typically not removed in most device replacement procedures as there are potential risks and complications. However, a doctor may recommend this for specific cases. If a doctor decides to remove leads, they will discuss why this procedure is necessary prior to performing it.

After a heart device is implanted, the implant site may be tender or swollen during recovery. Keep the area clean and watch for any signs of infection.
Consult with a doctor if experiencing any lingering pain or soreness.

Traditional heart devices are implanted on the left or right side of the chest, just below the collarbone. Some devices are unique and may be directly implanted into the heart, such as leadless pacemakers.

Higher intensity activities or movements that can cause strain on the body are cause for restrictions post-implant. Actions that involve pushing, pulling, or lifting heavy objects, exercising, and stretching are advised against for multiple weeks following the procedure. Consult with a doctor to address any questions and to develop a timeline for safely returning to these activities.

Lead dislodgement doesn't happen often, but it is possible. If a lead dislodges, it typically occurs shortly after implant, and will require the lead to be repositioned.

Depending on an individual's health situations, it is possible to carry over leads from a previously used device into a new one but there are many considerations for this to happen. Talk a doctor, who can advise on individual situations.


Typically, this will be a cardiologist or electrophysiologist, as they are the most common types of doctors specializing in the heart.

Talk to a doctor about any questions or concerns regarding medications.

Some heart devices have alert tones or vibrations and others do not. Typically, only an implantable cardioverter defibrillator (ICD) makes noise or vibrates, but some newer pacemakers have audible alerts. Talk to a doctor to learn more about individual devices and the possible tones they could emit.

Heat and humidity do not interfere with heart devices, but hot tubs may affect people with certain medical conditions. Discuss this with a doctor.

These systems should not affect your heart device. However, as a precaution, do not linger near or lean against such systems. Walk through these systems at a normal pace. If you are near such a system and experience symptoms, promptly move away from the system. After you move away, the heart device resumes its previous state of operation.

Most people who have received an ICD shock describe the event in a unique manner. It is normal to feel apprehensive, but also remember that a defibrillating shock from an ICD can be lifesaving. For most people, if there is pain, it quickly passes.

A roller coaster won't affect an implanted heart device but check with a doctor to make sure there are no heart conditions that prevent riding. A roller coaster may have shoulder bars that can rest uncomfortably on a device. Items such as additional padding, an extra shirt, or towel can be used to protect the devices in these cases from rough, physical contact to the implant site.
Additionally, keep a heart device at least 6 in (15 cm) away from any magnetic components.
The heart is roughly the size of a fist and sits in the middle of the chest, slightly to the left. Each day, the heart beats approximately 100,000 times and is the center of the circulation system, pumping blood throughout the body. This blood delivers oxygen and nutrients to all parts of the body to help organs and muscles work properly.
The sensation will differ for each individual patient. A shock from an ICD can feel like a sharp or quick thump to the chest. The muscles in your chest and upper arm may tighten so strongly that you jump up in surprise. Try not to worry if this happens, remember that a defibrillating shock from an ICD can be lifesaving. If there is any pain caused by a shock, it often passes quickly. Anyone touching you at the time you get the shock may feel a muscle spasm or a tingle. It will not hurt the person touching you. Any questions on what to expect in the event of a shock should be directed to your doctor.

There are potential symptoms to identify something is interfering with a heart device, like shortness of breath, dizziness, sudden weakness, fluttering in the chest, lightheadedness, fainting, or possibly an inappropriate shock. Generally, moving away from the item that is causing the interference will resolve the issue. Talk to a doctor to discuss further.
Answers are generated for generic purposes and products may not be suitable for everyone. Product suitability and therapies should be discussed with a Healthcare Professional
The information provided on the site is for educational purposes only, and does not substitute for professional medical advice.
You just clicked a link to go to another website. If you continue, you will leave this site and go to a site run by someone else.
Medtronic Canada does not review or control the content on the other website, and is not responsible for any business dealings or transactions you have there. Your use of the other site is subject to the terms of use and privacy statement on that site.
It is possible that some of the products on the other site not be licensed for sale in Canada.